Lymphedema is a chronic condition that causes swelling in your arms, legs, or other parts of your body. There’s no cure, but lymphedema responds well to treatment when you use the right approach.
So, what is the most effective treatment for lymphedema? The answer is Complete Decongestive Therapy. This approach addresses swelling through multiple techniques that all work together.
As a certified lymphedema therapist (CLT-LANA), I often see lymphedema patients in my clinic who haven’t learned about the options available to help them manage their swelling and improve their quality of life.
So, in this article, I’ll share the most effective ways to treat lymphedema.
What Is Lymphedema?
Lymphedema is a medical condition in which lymph fluid accumulates in your body’s tissues, usually in an arm or a leg. This causes swelling, along with feelings of heaviness, tightness, or discomfort.
Some people are born with lymphatic system problems that lead to swelling (primary lymphedema). But most cases develop after something damages the lymphatic system, such as cancer treatment, surgery, radiation, infection, or injury (secondary lymphedema).
Research shows that 1 in 30 people live with lymphedema worldwide.
Without treatment, lymphedema typically gets worse over time. The swelling increases, your skin and tissues can harden and thicken, and moving the affected arm or leg becomes more difficult. You also face higher risks of skin breakdown, wounds, and serious infections.
Sometimes, lymphedema develops in less common areas of the body. For example, there is neck lymphedema and genital lymphedema, but they’re less common than arm or leg lymphedema.
Can You Treat Lymphedema?
Yes. Lymphedema is chronic, but it’s treatable.
As a certified lymphedema therapist and physical therapist, I regularly see patients who’ve been living with swelling for years without realizing they had options to improve it.
They’ve often been told it’s something they just have to live with, or they’ve never been connected with someone who could teach them how to manage it.
You can’t cure lymphedema because the underlying damage to your lymphatic system is permanent. However, you can control the swelling, reduce discomfort, and maintain normal function with the right treatment.
In early-stage lymphedema, some people can even eliminate visible swelling completely, though the lymphatic damage remains.
At the same time, without consistent treatment, lymphedema can become dangerous because it makes you more susceptible to serious skin infections.
What Is the Most Effective Treatment for Lymphedema?
The gold standard treatment for lymphedema is Complete Decongestive Therapy, also called CDT. This is a comprehensive, non-invasive approach that works through two distinct phases.
Phase 1 is the intensive treatment phase. It typically lasts 2 to 6 weeks, and you work closely with a certified lymphedema therapist several times per week. This phase includes:
- Compression bandaging with multiple layers
- Manual lymphatic drainage (a specialized massage technique)
- Exercise
- Skin care
The goal during Phase 1 is to reduce your limb size and swelling as much as possible.
Once your swelling has decreased to its maximum level, you move into Phase 2. This is the long-term maintenance phase where you learn to manage your lymphedema at home.
Phase 2 includes:
- Daytime compression garments
- Nighttime compression garments or bandaging
- Exercise
- Skin care
- Other lymphedema self-care techniques
Complete Decongestive Therapy combines all these components because they work best together. However, everyone’s lymphedema is different, so the specifics of your treatment plan may look different from someone else’s.
Let’s take a closer look at each part of treating lymphedema:
Compression Bandaging
Compression bandaging is one of the most effective ways to reduce lymphedema swelling.
These bandages are called short-stretch bandages, and your therapist applies them in multiple layers using cotton padding and foam padding to gradually shrink the size of your affected limb.
They might look like ACE bandages, but they work differently.
Research shows that compression bandaging is the most critical factor in reducing limb size during CDT. Some studies even found that bandaging alone works just as well as bandaging combined with other Phase 1 treatments.
Because proper bandaging technique is so important for both effectiveness and safety, you need to work with a certified lymphedema therapist. They’ll show you which foams and paddings work best for softening your skin and protecting your limbs.
Compression Garments
Compression garments are special sleeves or stockings that support your lymphatic system and encourage lymph fluid drainage.
If you have mild swelling, compression garments alone might reduce it. For moderate to severe lymphedema, garments work as maintenance tools. They keep swelling from coming back after you’ve reduced it through Phase 1 treatment.
You’ll be sized and fitted for garments after you complete the intensive treatment phase.
Wearing the wrong type of compression garment won’t help treat your lymphedema, and with so many options available, figuring out what you need can feel overwhelming. Here are the main categories:
Circular Knit Garments
These garments are elastic and typically come in standard sizes you can buy off the shelf. The most common medical-grade compression level is 20-30 mmHg, though you can find different strengths.
Circular knit garments work well for mild swelling, but they’re not effective for moderate or severe lymphedema.
Flat Knit Garments
These garments are inelastic and usually custom-made to fit your exact measurements. A few brands offer pre-sized options, like the Solaris Exostrong stockings and armsleeves.
Flat knit garments are the best choice for moderate to severe lymphedema because they do a better job of preventing swelling from returning.
The fabric is thicker than circular knit, which can make these garments harder to put on. However, there are tools and techniques that make donning them much easier.
To get fitted for custom flat knit garments, you’ll need to work with a local fitter who can take your measurements and help you choose the right brand and style.
Velcro Wraps
Velcro wraps are another option for compression. They’re typically not as effective as flat knit garments, but they can be easier to put on and take off independently.
If struggling with garment application keeps you from wearing compression consistently, velcro wraps might be a good solution. Here’s a tutorial on how to put on compression socks.
Nighttime Garments
Nighttime garments are an alternative to compression bandaging in the evenings. Some are custom-made (like the L&R Tribute), and others come ready-to-wear with velcro straps, or as padded liners you can bandage over.
These garments save time with your evening routine and provide skin care benefits through built-in foam chips that help soften thickened tissue or fibrosis.
Manual Lymph Drainage
Manual lymphatic drainage, or MLD, is a massage technique that helps move lymphatic fluid out of swollen areas and back into your lymph vessels, where it can drain.
The technique uses very light pressure to gently brush and stretch your skin in specific sequences and directions. You can also learn to do it at home with your doctor’s approval:
MLD is a standard part of Complete Decongestive Therapy, but research shows mixed results about how well it works.
Some studies found that MLD helps reduce mild lymphedema but doesn’t do much for severe swelling. One study even showed that combining MLD with compression bandaging wasn’t more effective than bandaging alone. However, other studies found that MLD does reduce fluid buildup and swelling.
In other words, MLD should remain a treatment option, but what works best varies from person to person.
You might need to try MLD for yourself to see if it helps your symptoms. However, in my practice, many people living with lymphedema find this type of lymphatic therapy/massage therapy very helpful.
See this before and after of lymphatic drainage massage.
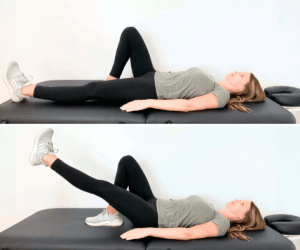
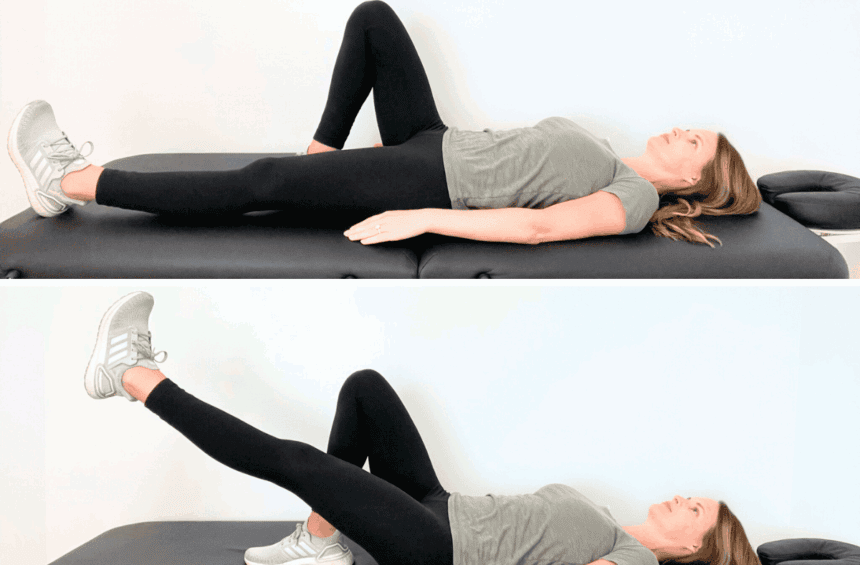
Exercise
Exercise and movement are essential for managing lymphedema. Your muscles act as a pump for both your lymphatic system and your veins.
When you contract and stretch your muscles, you help move fluid through your vessels.
Popular exercise options for lymphedema include cardio exercise in the pool, gentle aqua movements, walking, and rebounding exercises using a mini trampoline. Some people also find vibration plates helpful.
Overall, the best exercise for lymphedema is whatever you enjoy and can do consistently.
Learn more about vibration plates vs. rebounders.
Skin Care
The final component of Complete Decongestive Therapy is skin care.
Your skin is your main defense against bacteria and infection. When you have lymphedema, your immune system doesn’t work as well in the affected area, which makes protecting your skin even more important for your overall health.
Keeping your skin clean, moisturized, and protected from cuts, scrapes, and irritation helps prevent infections like cellulitis that could make your lymphedema worse.
Healthy Habits
Beyond the core components of CDT, healthy lifestyle habits can help improve your lymphedema symptoms.
Losing weight if you’re carrying extra pounds, eating a balanced diet, and staying generally active all support better lymphedema management.
In my practice, I’ve seen some people with lymphedema who have started using GLP-1 medications (like Ozempic or Wegovy) for weight loss to help manage swelling.
But it’s important to remember that these medications don’t repair the underlying lymphatic damage or cure lymphedema. They may help reduce swelling through weight loss, but you’ll still need to maintain your regular lymphedema treatment routine.
You may also find red light therapy for lymphatic drainage helpful.
Lymphedema Treatment: Phase 1 vs Phase 2
Phase 1 and Phase 2 of Complete Decongestive Therapy use many of the same tools, but they’re different.
Both phases use compression, lymphatic drainage, exercise, and skin care, but Phase 1 focuses on reducing swelling with professional help. Phase 2 is something you’ll do at home for the rest of your life to maintain those results through self-care.
Are There Surgical Treatments for Lymphedema?
Complete Decongestive Therapy has been around for decades and remains the gold standard treatment for lymphedema. However, surgical options are becoming more available, and they can also be beneficial in certain situations.
Three main types of lymphedema surgery exist:
- Lymphovenous anastomosis (LVA): Surgeons create a bypass by connecting lymphatic vessels directly to small veins in your affected limb, allowing trapped fluid to drain into your bloodstream.
- Vascularized lymph node transfer (VLNT): Healthy lymph nodes are taken from an unaffected area of your body and transplanted into the swollen area to restore lymphatic drainage and promote new vessel growth.
- Suction lipectomy: Surgeons remove excess fatty and fibrotic tissue that has built up in the affected limb, reducing its size.
Surgery can improve lymphedema symptoms, but it’s not a cure.
You’ll still need to wear compression garments and do other parts of your lymphedema self-care routine after the surgery, but you may have less excess fluid to manage.
That said, new surgical techniques and treatment options continue to emerge each year, bringing hope for better management strategies and potentially a cure in the future.
FAQs
What is the drug of choice for lymphedema?
No drug treats or cures lymphedema. It doesn’t respond to medication (at least yet), but you can manage the condition through compression, manual drainage, exercise, and skin care. All of these approaches are part of Complete Decongestive Therapy, which is the gold standard treatment for lymphedema.
Your doctor will likely have to prescribe antibiotics if you develop a skin infection, such as cellulitis, which is a common complication of lymphedema. But these drugs don’t treat lymphedema.
What kind of doctor treats lymphedema?
Usually, you’ll see a certified lymphedema therapist (CLT-LANA) for lymphedema treatment. This doctor is usually a physical therapist, occupational therapist, or massage therapist with specialized training in lymphedema management.
Learn more about the doctors who treat lymphedema, such as vascular surgeons or plastic surgeons, if you decide to go down the surgery route.
What complications can arise from lymphedema?
Unfortunately, lymphedema can trigger a few serious complications if left untreated. The most common is cellulitis, a bacterial skin infection that causes redness, warmth, pain, and fever.
Without proper treatment, lymphedema will most likely get worse over time. You’ll deal with more swelling, and your skin and tissues can harden and thicken (fibrosis). All of this negatively impacts your mobility and quality of life.
But the good news is that early treatment and consistent management will help prevent most lymphedema complications and allow you to live a full, active life.
Physical Therapy to Reduce Lymphedema Symptoms
Many people living with lymphedema don’t have access to a certified lymphedema therapist in their area. This leaves them without the education and treatment they need to manage their condition, even though lymphedema responds well to proper care.
If you’re struggling to find local lymphedema treatment or want guidance you can follow at home, I created online resources to help, all based on my experience as a certified lymphedema therapist (CLT-LANA):
- Lower Body Lymphedema Rehab for managing leg, foot, and lower body swelling
- Breast Cancer Rehab for arm lymphedema and upper body swelling, especially after cancer treatment
- Digital guides with exercises and management techniques you can do at home
All of these resources teach you the techniques used in professional lymphedema therapy so you can take control of your symptoms at home.