Scar tissue formation is a natural part of the healing process after a mastectomy. But scar tissue pain years after mastectomy isn’t normal or something you have to live with.
There are steps you can take to soften the scar tissue, relieve discomfort, and improve your quality of life.
Everyone’s healing timeline is different, but even small changes in treatment can lead to big results. As an oncology physical therapist, here’s what I recommend doing to reduce post-mastectomy pain around the scar.
Why Does My Mastectomy Scar Hurt?
After breast cancer surgery, your body makes scar tissue as part of healing. When your skin is damaged, your body produces collagen fibers to repair the wound. Sometimes your body makes too much collagen, which creates a scar.
Scar tissue isn’t as flexible as normal skin.
This makes the area feel tight or restricted. It can hurt when you lift your arm or make other movements that stretch the scar. The scar tissue can also get thicker over time or stick to nearby muscles and tendons, which makes the pain and movement restrictions worse.
Post-mastectomy pain syndrome around the scar is unfortunately common.
One study found that only 14% of mastectomy patients said their surgical scars had minimal or no negative impact on their lives.
Learn more about breast cancer rehabilitation.
Is It Normal for Scar Tissue to Hurt Years Later?
No.
It’s common for scar tissue to hurt even years after a mastectomy, but that doesn’t mean that chronic pain is normal.
As scar tissue matures and changes over time, it can cause discomfort. The tissue may tighten, pull on surrounding areas, or develop adhesions (where the scar sticks to muscles or other tissue underneath).
These changes can create new pain or make existing pain worse, but it doesn’t mean that breast cancer survivors should just accept this recurring pain as their new normal.
If you experience scar tissue pain after breast cancer treatment, there are steps you can take to minimize the symptoms and reduce discomfort.
As an oncology physical therapist, I regularly work with patients to help them break up scar tissue and get back to their daily activities without pain.
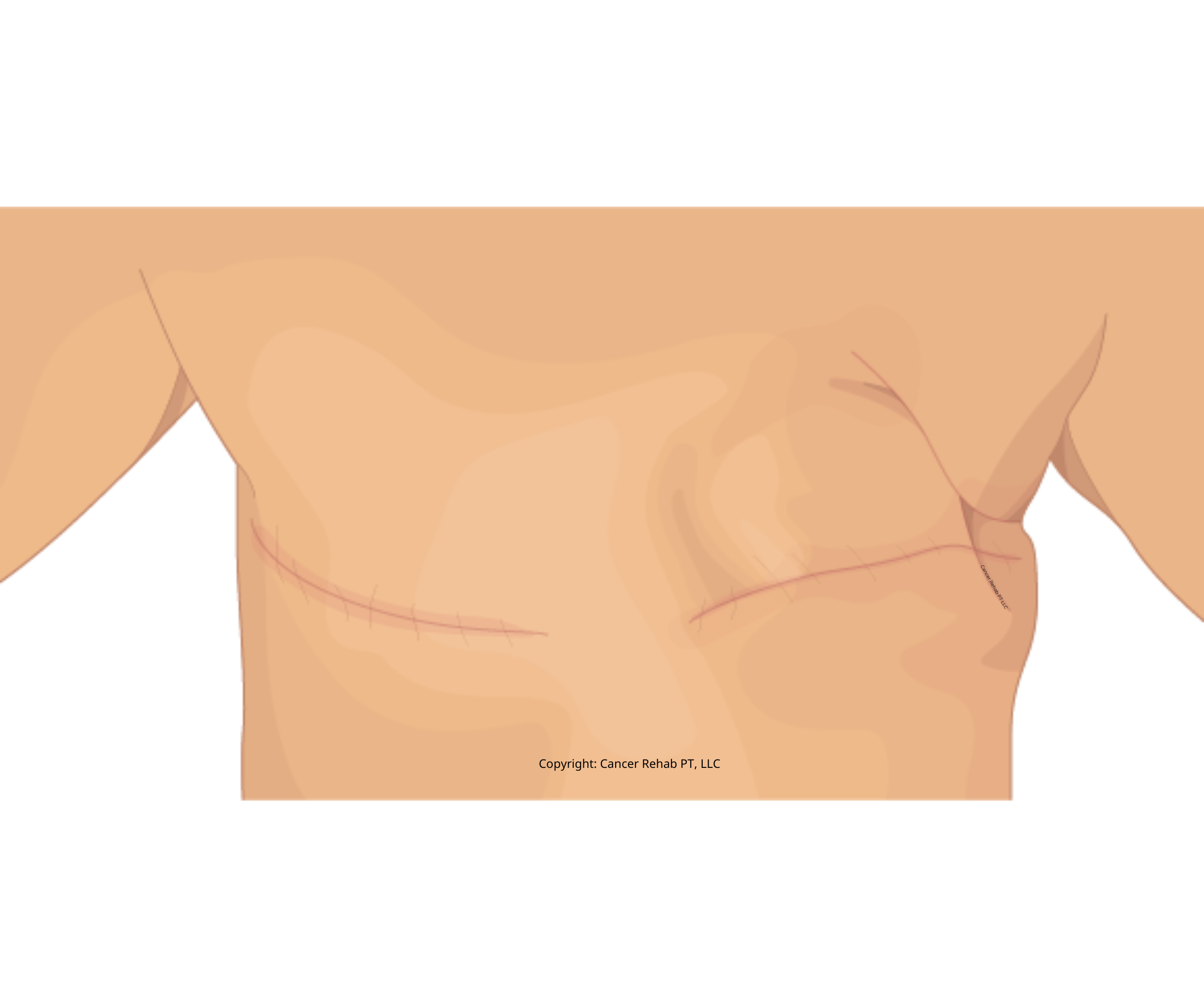
What Does Scar Tissue After Mastectomy Look Like?
Scar tissue after a mastectomy usually looks like a raised, thickened area of skin where your surgery was. It’ll also vary based on how your body heals and what surgical technique your surgeon used.
Right after surgery, the scar tissue may look red or pink.
Over time, it gradually fades to a lighter color. Some discoloration is common as your skin heals, and you might notice changes in pigmentation around the scar.
Your scar’s appearance will likely improve over time as the collagen matures and your skin becomes more flexible.
Mastectomy scars never completely disappear, but they usually become much less noticeable.

Risk Factors for Scar Tissue Pain after Breast Surgery
There are a few factors that can influence scar tissue formation and pain after breast cancer surgery or a prophylactic mastectomy.
That said, every person is different, and having some of these risk factors doesn’t necessarily mean that you’ll develop pain after breast surgery.
Here’s what I see in my practice:
Surgical Technique
The method your surgeon uses can affect how much scar tissue forms.
Surgeries that involve more tissue trauma or larger incisions may create more extensive scarring (for example, mastectomies that involve lymph node removal or axillary lymph node dissection).
Infection
Infections at the surgical site can slow down the healing process and lead to excessive scar tissue.
To avoid infections, make sure to keep your surgical scar clean and change the dressing as recommended by your surgeon.
Genetics
Your genes play a role in how your body heals, and some people are simply more prone to scarring after breast cancer treatment and breast reconstruction.
Age
Older adults may develop more extensive scar tissue because of natural skin changes that happen with age.
Radiation Therapy
If you have radiation therapy after your mastectomy, you may be at higher risk for scar tissue pain. Radiation affects the skin and underlying tissue, which can increase scarring.
Health and Lifestyle
Your overall health matters, too.
People with chronic conditions like diabetes or immune system disorders, those in poor health, and smokers are more likely to have ongoing scar tissue pain and cording after a mastectomy.
How to Break Up Scar Tissue After Mastectomy: 6 Ways to Reduce Pain and Heal
If your scar tissue is painful and bothering you, there are ways to manage it with physical therapy and self-care.
As an oncology physical therapist, here are some of my favorite things to do to reduce breast tissue pain after a mastectomy, even if it’s been years since your surgery.
You can also follow this Breast Cancer Recovery Roadmap.
1. Keep It Clean
Keeping the area around your scar clean helps prevent infections and supports healing.
Wash the area gently with mild soap and water. Don’t scrub hard because that can irritate your skin, and make sure to completely dry it after.
2. Moisturize
Moisturizing your scar regularly helps make it softer and more flexible.
Use a gentle, fragrance-free moisturizer and rub it on your scar in small circles.
You can use petroleum jelly or Vaseline, but I also like Vitamin E Oil and a Silicone Gel to decrease scarring. These create a protective layer over the scar and help prevent scabbing.
Avoid products with lots of chemicals, alcohols, and fragrances. The simpler the ingredient list, the better, because chemicals can irritate your scar and make the pain worse.
I recommend this Natural Vitamin E Oil and Silicone Scar Sheets.
3. Scar Tissue Massage
Massaging your scar tissue can make it thinner and help your skin move more easily. The basic idea is to gently pick up and roll the scar tissue between your fingers.
This helps break down the scarring and soften the area.
Ask a physical therapist or your medical team to show you how to start, or you can also learn how to do this by following my YouTube video:
4. Soft Tissue Mobilization (STM)
Soft tissue mobilization is a technique that works on the deeper tissues under your skin to reduce tightness and discomfort. Sessions should take 15-30 minutes, followed by 10-15 minutes of stretching.
You can find detailed demonstrations of these techniques in my program Breast Cancer Rehab.
You can do this at home, but get your doctor’s approval first. Your incisions should be completely healed, and make sure your hands are clean to avoid infection.
5. Use Sunscreen
It’s important to protect your scar from the sun to prevent discoloration and help it heal better. Sun exposure can cause your scar to darken or develop uneven color.
Put SPF 30 (or higher) sunscreen on your scar whenever it’s exposed to the sun. This prevents further skin damage and keeps your scar from getting darker.
6. Active Stretching
Adding stretching exercises to your daily routine helps improve flexibility and movement around your scar.
Do gentle stretches for your chest, shoulders, and arms to prevent stiffness and keep the scar from sticking to tissue underneath.
Stretching increases blood flow to the area, which softens the tissue and reduces pain after breast cancer surgery. In fact, according to BreastCancer.org, physical therapy is one of the main ways to manage or improve scar tissue pain.
If you want to try gentle yet effective exercises after a mastectomy, I have a few handy guides that you may find helpful, in early-stage breast cancer recovery, as well as years after treatment:
FAQs
Can scar tissue cause pain 10 years later?
Yes, scar tissue can cause pain even a decade or more after your surgery. Over time, scar tissue can tighten, develop new adhesions, or respond to changes in your body like weight fluctuations or hormones. Old scar tissue can also become irritated from repetitive movements or new injuries to the area. However, just because years have passed doesn’t mean the pain can’t be treated, and physical therapy can help at any point after the surgery, even with severe pain or nerve pain.
Can scar tissue turn cancerous?
No, scar tissue can’t turn into cancer. It’s made of collagen fibers that form during healing, so it’s not something that can become cancerous, although many breast cancer survivors worry about this. However, it’s important to monitor any changes in your scar or the surrounding area. If you notice new lumps, changes in texture, unusual pain, or other concerns, contact your doctor.
What does mastectomy scar tissue feel like?
Mastectomy scar tissue can feel different for everyone. You might feel tenderness and sensitivity around the area, especially at first. As the scar matures, it often feels thick and firm, and can cause a pulling or stretching feeling. Many people describe it as a dull ache or pressure, especially when moving their chest or shoulder. The scar may also feel raised or lumpy when you touch it.
Learn more about double mastectomy recovery time and what to expect in terms of your scar.
How do you break up scar tissue after a mastectomy?
You can break up scar tissue using techniques like scar tissue massage, soft tissue mobilization, and active stretching. These methods help soften the scar, improve movement, and reduce pain. Scar tissue formation is natural after surgery, but it doesn’t have to come with feelings of tightness or pain. Mild discomfort and increased sensitivity are expected at first, but they should be getting better over time.
Should I massage my mastectomy scar?
Yes, massaging your scar can help with healing and discomfort. When done gently and correctly, scar massage breaks down adhesions, improves blood flow, and makes the tissue softer and more flexible. But check with your doctor or physical therapist before you start to make sure it’s safe for your situation. They can also show you the right technique to use.
How long do mastectomy scars take to fade?
It varies from person to person based on your healing process, skin type, and surgery details. Most scars become less noticeable within the first year. However, complete fading can take several years, and some scars may always have some discoloration or texture changes. Using sunscreen consistently and following proper scar care helps minimize pigmentation changes and supports better healing.
How do you know if pain is from scar tissue?
Scar tissue pain usually feels tight, pulling, or achy around your surgical area. It often gets worse with certain movements, especially ones that stretch the chest or shoulder. The pain might feel like it’s coming from just under the skin or deeper in the tissue. If you press on the scar area, it may feel tender, or you might feel tight bands under the skin. The location and timing of the pain are usually the biggest cues.
Do I Have to Accept Scar Tissue Pain Years After Mastectomy as Normal?
No, you don’t have to live with pain as part of your daily life after breast cancer surgery. There are techniques and self-care practices that can break up scar tissue, reduce limitations, and help you heal.
As a Doctor of Physical Therapy and a Board-Certified Oncology Specialist, I’ve helped hundreds of patients reclaim control and improve their quality of life after breast cancer.
However, I know that it can be hard to see a physical therapist in person because of location or costs.
This is why I created Breast Cancer Rehab, an online program that teaches you the same knowledge and techniques I share with my patients at the physical therapy clinic.
There’s a full module inside the program dedicated to managing scar tissue pain, but you’ll also find helpful physical therapy exercises to help with swelling, arm mobility, cording, and more.
Learn more about Breast Cancer Rehab and join!