Axillary Web Syndrome (AWS), also called cording, is a common side effect of breast cancer surgery and lymph node removal.
It happens when tight, rope-like cords form under your skin, usually starting in your armpit and sometimes running down your arm.
These cords can make it hard to lift your arm, and they can be painful. Even though AWS is common, it doesn’t get talked about enough, and many people don’t realize there’s something they can do about it.
But cording is treatable. With physical therapy, you can reduce pain, regain your mobility, and get back to your normal life.
What Is Axillary Web Syndrome (Cording)?
Axillary Web Syndrome often develops after breast cancer surgery or lymph node surgery, with some studies reporting rates as high as 86%.
Some things can increase your chances of getting AWS, such as a higher number of lymph nodes removed or more extensive breast cancer surgery.
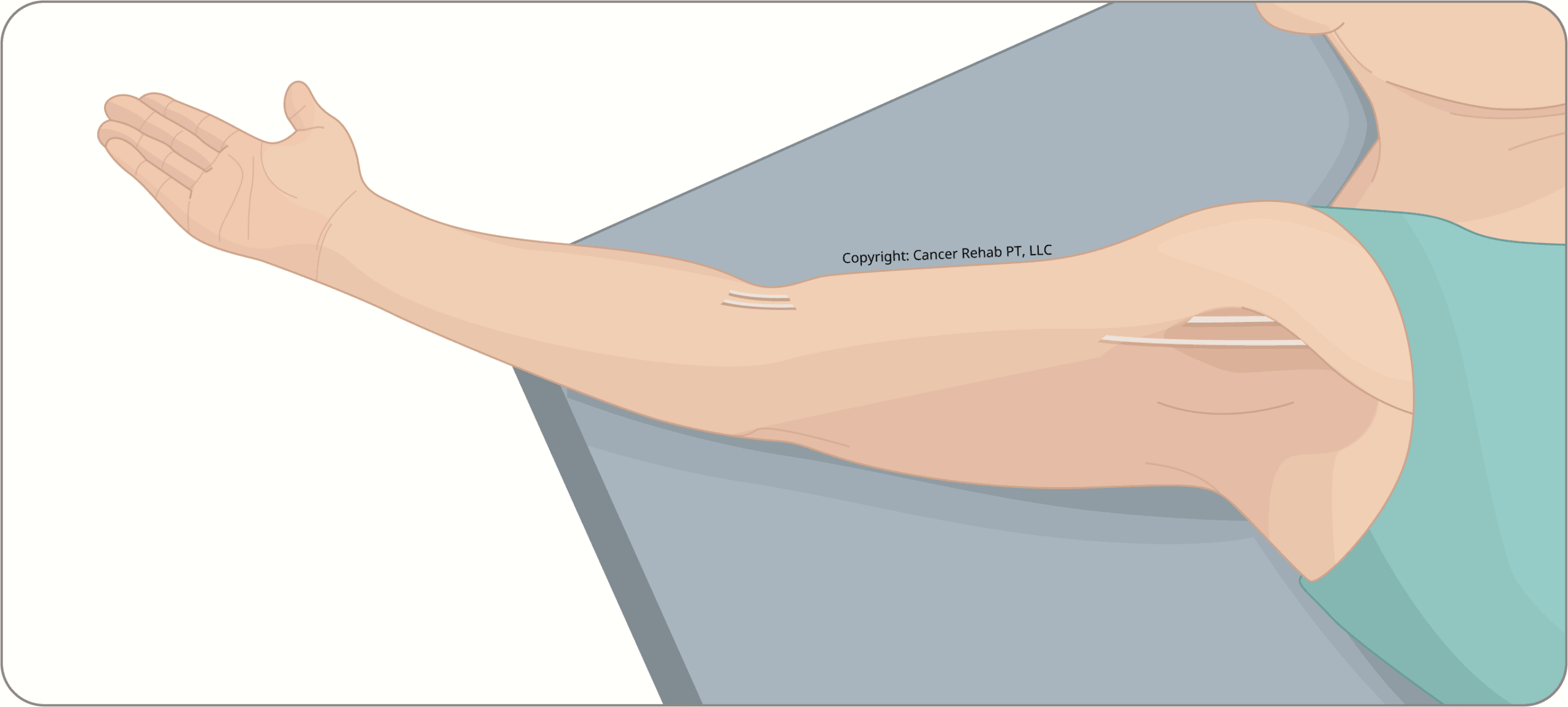
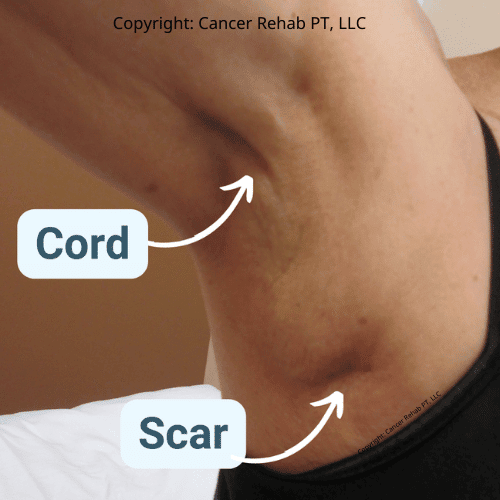
Cords are exactly what they sound like.
They are thin, guitar cord-like structures that can run from the armpit all the way down to the wrist in some cases.
You can have multiple small cords or one single long and tight cord. Many cords aren’t visible on the surface, so even if you don’t see the cords in your armpit or upper arm, you may still have invisible axillary cord formation.
The signs and symptoms of Axillary Web Syndrome can include:
- Mild discomfort
- Severe pain
- Feeling of tightness
- Visible or palpable cord-like structures under the skin
Cords typically show up 2 to 8 weeks after surgery, but in some cases, they can appear weeks or even months later. Some cords can go away on their own, but some may require management strategies and physical therapy treatment.
Cording doesn’t have to be permanent. I often see people in my physical therapy practice who manage and improve AWS relatively quickly with the right knowledge and care.
Learn more about the 5 things they never tell you about life after cancer.
Axillary Web Syndrome Causes
Researchers don’t know the exact cause of AWS, but it’s linked to how your body heals after surgery or radiation.
When you have surgery in your armpit area, such as a lumpectomy or a mastectomy, your body responds with inflammation.
This inflammation can damage small blood vessels and lymph vessels, which then harden into the fibrous cords you feel under your skin.
Essentially, you can think of it as scar tissue forming in thin lines instead of a flat patch.
Lymph Node Removal and AWS Risk
What researchers DO know is that one of the biggest factors in AWS development in breast cancer patients is how many lymph nodes were removed during the surgery.
There are two main types of surgeries in breast cancer treatment that remove lymph nodes:
- A Sentinel Lymph Node Biopsy (SLNB) removes 1 to 5 lymph nodes to check whether cancer has spread. It’s less invasive, but it can still lead to cording.
- An Axillary Lymph Node Dissection (ALND) removes more than 5 lymph nodes and comes with a higher risk of AWS.
If you’ve had either of these axillary surgeries, I recommend knowing what to watch for.
Even if you do develop Axillary Web Syndrome, many people see big improvements in their symptoms within 8 to 16 weeks after surgery with the right treatment.
To speed up your recovery, follow this Breast Cancer Recovery Roadmap.
Can You Get Axillary Web Syndrome Without Surgery?
Yes, though it’s less common.
AWS can develop after radiation therapy, even without lymph node surgery. It can also show up after other procedures in the armpit area, like port placement or removal.
It’s not just breast cancer survivors who develop cording.
If you’re experiencing that tight, cord-like feeling in your armpit or down your arm and you haven’t had lymph node surgery, I recommend getting evaluated.
The treatment approach is the same, whether AWS developed as a result of a procedure like a sentinel node biopsy or for other reasons.
Cording Is Not Something You Have to “Learn to Live With”
Axillary Web Syndrome is a manageable condition, and it often resolves within ~3 months with the right treatment and exercises.
Physical therapy is what I recommend as the primary treatment for cording. It involves:
- Educational resources
- Physical therapy exercises
- Stretches and neural mobilization (nerve glides)
The main strategy is to stay proactive.
Regular exercises and techniques can help you manage AWS effectively, reducing arm limitations and pain. You may feel better after just a few therapy sessions.
These exercises after a mastectomy can help, too.
Axillary Web Syndrome Treatment
Treatment for AWS focuses on breaking down the tight cords, restoring your range of motion, and managing pain.
Most people respond well to physical therapy treatment, but you may also benefit from laser therapy and pain medications when needed.
Physical Therapy
Physical therapy is the most effective treatment for cording symptoms.
PT for AWS typically includes hands-on techniques like manual therapy and soft tissue mobilization to help loosen the cords, plus targeted stretches and exercises to restore your range of motion.
Your therapist may also use nerve glides to improve mobility and break down scar tissue, and they’ll give you a home exercise program so you can continue making progress between sessions.
As a physical therapist, I often use these exercises and stretches in my practice:
- Sidelying pec stretches
- Corner or doorway stretches
- Nerve glides (also called nerve flossing)
- Shoulder flexion and abduction exercises
- Scar tissue mobilization techniques.
These strength and stretching exercises gradually lengthen the tight cords, reduce pain, and get your arm moving freely again.
If you’re dealing with cording, I’d encourage you to find a physical therapist who has experience with breast cancer rehab.
As an oncology PT, I also often see AWS in my clinic, and I created a few resources that you may find helpful:
Learn more about breast cancer rehabilitation and the role physical therapy plays in it.
Laser Therapy
Some physical therapists use low-level laser beams to help break down thickened scar tissue.
It can reduce pain and improve flexibility, though results vary depending on how severe your cording is. This is something to discuss with your PT if other treatments aren’t giving you enough relief.
Medication and Pain Management
Over-the-counter NSAIDs (nonsteroidal anti-inflammatory drugs), such as ibuprofen, can help with pain and inflammation as you’re working through your physical therapy treatment plan.
If your pain is more severe, talk to your doctor about whether a prescription option makes sense for you.
Axillary Web Syndrome Without Cancer
Axillary Web Syndrome is most common with a breast cancer diagnosis, but it can happen in other situations, too.
Any surgery or procedure that affects the armpit area can potentially cause cording, including port placement or removal, surgery for melanoma, and other surgeries where lymph nodes in the armpit are biopsied or removed.
Radiation therapy to the chest or armpit can also lead to AWS, even without surgery.
If you’re experiencing tight cords in your armpit or down your arm after any kind of procedure in that area, it’s worth getting evaluated.
You’ll need physical therapy to treat Axillary Web Syndrome and make the hardened scar tissue more flexible, no matter what caused it.
FAQs
Is Axillary Web Syndrome dangerous?
Axillary Web Syndrome isn’t dangerous, but it’s often painful and limiting. The cords themselves don’t pose a health risk. They’re not a sign of infection or cancer spreading, and they don’t affect your life expectancy. But they do have a big impact on your quality of life because of the restricted arm movement, discomfort, and difficulty with everyday tasks like reaching overhead or getting dressed.
Is Axillary Web Syndrome a sign of cancer?
No, Axillary Web Syndrome isn’t a sign that cancer has returned or spread. It’s an unfortunate side effect of surgery or radiation therapy, especially if these procedures involved your lymph nodes. The cords form because of how your body heals after trauma to the armpit area. It’s scar tissue and inflammation, not cancerous tissue.
Does Axillary Web Syndrome go away?
Yes, in most cases, but it’s important to take action to help your body heal instead of waiting for the cording to go away on its own. Some cords do resolve on their own after a few weeks, but many invisible and visible cords take much longer and need physical therapy to go away.
What are the symptoms of Axillary Web Syndrome?
The main symptom is a tight, cord-like band under your skin, usually starting in your armpit. It can extend down your inner arm, sometimes reaching your elbow or wrist. You might feel pain or pulling when you try to lift your arm, reach overhead, or straighten your elbow.
Some people can see or feel the cord clearly, but it’s also possible to just notice tightness and restricted movement without a visible cord.
How do you fix Axillary Web Syndrome?
Physical therapy is the most effective treatment for Axillary Web Syndrome. A PT who specializes in oncology rehab can use manual therapy, stretching, and nerve glides to loosen the cords and restore your range of motion. You’ll also get exercises to do at home. In some cases, low-level laser therapy or anti-inflammatory medication can help, too.
What does axillary cording look like?
Cording looks like a thin, tight rope or string running under your skin. It usually starts in your armpit and can extend down the inside of your upper arm. When you lift your arm or stretch, the cord may become more visible, and it can look like a guitar string pulling just beneath the surface. Some cords are invisible, but they still cause discomfort.
Can AWS be prevented?
Sometimes, yes. Starting gentle movement and stretching exercises soon after surgery (once your doctor clears you) can help reduce your risk of developing cording. This is because early mobilization keeps the tissue from tightening up as it heals.
Learn more about double mastectomy recovery time.
What are the early signs of cording?
The earliest signs are usually tightness or a pulling sensation in your armpit when you try to raise your arm. You might notice you can’t lift your arm as high as before, or that reaching feels restricted. Some people feel a tender spot in their armpit before a visible cord develops. If you notice any of these symptoms in the weeks after surgery, let your care team know so you can start treatment early.
Get More Support in Breast Cancer Rehab
Physical therapy after breast cancer treatment is the main way to prevent and treat Axillary Web Syndrome.
But unfortunately, not everyone has easy access to physical therapy. Sessions can be expensive, oncology PTs aren’t available everywhere, and fitting appointments into your schedule isn’t always realistic.
That’s why I created Breast Cancer Rehab: an online program that gives you the same expert guidance I use with my in-clinic patients, in a format you can access from home on your own schedule.
The program includes in-depth education on what to expect during recovery, step-by-step exercise videos, and targeted modules for axillary web syndrome, scar tissue, arm mobility, lymphedema risk reduction, and more.
You can use it as your primary rehab resource or as a supplement to in-person PT sessions.
Learn more about Breast Cancer Rehab and join!